How to Understand Interlocking Nail Implant Benefits and Risks?
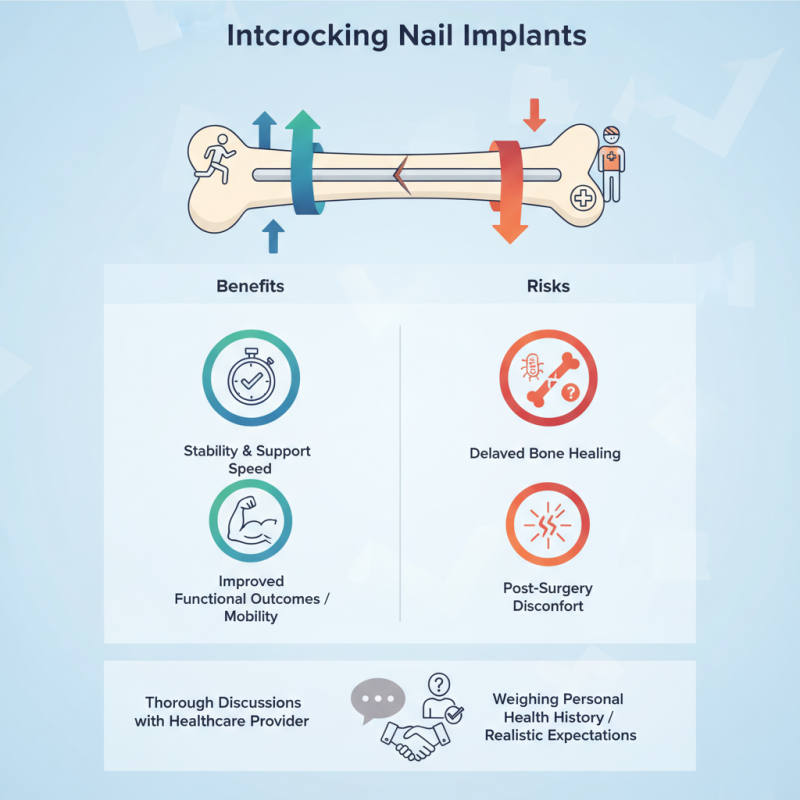
Understanding the benefits and risks of an Interlocking nail implant is crucial for patients considering this treatment. An interlocking nail implant is designed to provide stability and support during the healing process of long bone fractures. It can enhance recovery speed and improve functional outcomes. However, like any surgical intervention, it comes with potential complications.
Patients should be aware of possible risks, such as infection or delayed bone healing. Some might experience discomfort post-surgery. While many benefit from increased mobility, not everyone will have the same experience. Factors like age and overall health can affect results.
Additionally, the decision to use an interlocking nail implant should involve thorough discussions with a healthcare provider. This includes weighing personal health history against the procedure's advantages. A clear understanding of both sides promotes better patient outcomes and sets realistic expectations.
Understanding Interlocking Nail Implant: Overview of the Procedure
Interlocking nails are common in orthopedic surgery. This procedure stabilizes fractured bones, especially in long bones like the femur and tibia. Surgeons implant a metal rod through the bone, securing it in place. Studies show a 90% success rate in healing with this method. However, it's crucial to weigh the benefits and risks.
The advantages include immediate stability and reduced recovery time. Patients often experience less pain post-surgery. According to a 2021 report, over 80% of patients reported satisfaction with their interlocking nail procedure. Yet, complications can occur. Infection, improper alignment, or non-union of bones are potential risks. Surgeons need to evaluate each case carefully.
**Tips:**
Ensuring proper post-operative care is essential. Regular follow-ups help detect any complications early. Pay attention to unusual pain or swelling. Engaging in physical therapy can enhance recovery. Always discuss concerns with your surgeon, as open communication is critical.
Understanding Benefits and Risks of Interlocking Nail Implants
This chart illustrates the benefits and risks associated with interlocking nail implants. The data indicates that the patient satisfaction rate is relatively high at 85%, while the infection risk is low at 5%. The average fracture healing time is approximately 12 weeks, while the reoperation rate stands at 10%. These statistics can help patients and healthcare providers better understand the implications of this procedure.
Benefits of Interlocking Nail Implants for Bone Fracture Treatment
Interlocking nail implants are widely used in bone fracture treatment. They offer significant stability and allow for early mobilization. This is crucial for recovery. Studies suggest a success rate of over 90% for complex fractures. These implants help in maintaining alignment during healing.
Patients often report less pain and faster recovery times. A report from the American Academy of Orthopaedic Surgeons highlights that interlocking nails result in fewer complications compared to traditional methods. However, there are risks. Implant-related infections and non-union of fractures can occur. These issues require careful patient selection.
It is essential to understand that while the benefits are clear, not every case is ideal for interlocking nails. Surgeons must weigh the options carefully. Some patients may experience discomfort or complications long after surgery. Regular follow-ups are necessary to monitor healing and potential issues. Overall, interlocking nail implants can be beneficial but require thoughtful consideration.
Risks and Complications Associated with Interlocking Nail Implants
Interlocking nail implants are increasingly popular in orthopedic surgery. However, understanding their risks and complications is crucial for patients and healthcare providers. These implants can result in infections, which may require further intervention. The placement site can also experience significant pain, impacting recovery. Some patients may report discomfort long after surgery.
Tips to reduce risks include following post-operative care instructions closely. Keeping the area clean is vital. Discuss any unusual symptoms with your healthcare provider sooner rather than later. Regular follow-ups help catch potential complications early.
There’s also a risk of malalignment, where the nails do not align perfectly. This can lead to improper healing and functional issues. Patients may feel anxious about their recovery due to these risks. Consider joining support groups for shared experiences and encouragement during recovery. Engaging with others on the same journey can provide comfort. Understanding the benefits, alongside these risks, can empower patients to make informed decisions.
Patient Selection Criteria for Interlocking Nail Implant Procedures
Selecting candidates for interlocking nail implant procedures requires careful consideration. This method is often used for long bone fractures, particularly in the femur and tibia. Not all patients are suitable. Age, fracture type, and overall health play significant roles in decision-making.
Patients must also demonstrate a commitment to post-surgery rehabilitation. Those with substantial or complex fractures may face additional challenges. Compliance with treatment plans is crucial. If a patient has prior infections or is a smoker, this may increase the risk of complications.
Moreover, psychological readiness is essential. Patients must understand the procedure, potential outcomes, and risks involved. Clear communication with the surgical team can help align expectations. Decisions should always involve thorough discussions of benefits and drawbacks related to the patient's unique situation.
Post-Operative Care and Recovery After Interlocking Nail Implant Surgery
After interlocking nail implant surgery, proper post-operative care is crucial for recovery. Patients should closely follow their medical team's instructions. Medications for pain and inflammation may be prescribed. Swelling and discomfort are common but manageable. Using ice packs on the affected area can help relieve swelling.
Mobility may be limited initially, so patients should use crutches as directed. Gradually increasing activity levels is important. Physical therapy often follows the surgery. This aids in restoring strength and flexibility. It’s essential to attend all therapy sessions. Patients might experience moments of frustration during recovery. Remember, healing takes time and patience.
Infection is a risk after any surgery, so observant care is needed. Watch for signs like excessive redness, swelling, or fever. Regular follow-ups with your healthcare provider are vital. Discuss any concerns or unexpected changes. Accepting that recovery has ups and downs is part of the journey. Each step, even the setbacks, is a step towards healing.
